
Meloxicam, brands for which include Metacam and Meloxidyl, is a nonsteroidal anti-inflammatory drug (NSAID) that may be used in cats to reduce pain and inflammation. In this article you’ll learn how meloxicam works for pain management, when it is used in cats, precautions and adverse effects, and some frequently asked questions.
Meloxicam for Cats Overview

About Meloxicam for Cats

Meloxicam is a nonsteroidal anti-inflammatory drug (NSAID) used to treat pain and inflammation in cats.
Meloxicam is a COX-2 preferential nonsteroidal anti-inflammatory drug (NSAID). The most common brand, Metacam, is manufactured by Boehringer Ingelheim.
COX stands for cyclo-oxygenase. There are two main COX pathways in the body called COX-1 and COX-2. Both pathways involve enzymes that convert a large molecule called arachidonic acid into other components that have either protective or inflammatory effects on the body.
The COX-2 pathway is one primarily of inflammation where inflammatory mediators like cytokines trigger this pathway to create further mediators that cause more pain and inflammation.
The COX-1 pathway is very different, as its pathway is responsible for protective mechanisms, especially as they relate to the protective lining of the stomach, blood flow through the kidneys, and blood clotting.
Also Read: What To Do If Your Cat Is Sneezing Blood
Some NSAIDs act to block the COX-2 pathway but at the same time also block the COX-1 pathway. This leads to reduction of inflammation, but also greatly increases risk for ulceration and bleeding in the stomach and damage to the kidneys.
But there are also COX-2 selective or preferential NSAIDs, which means while they can affect both pathways, they have a much greater predilection for blocking the COX-2 pathway of inflammation, while leaving the protective COX-1 pathway alone.
There are also COX-2 specific medications, which only act on the COX-2 pathway while leaving the COX-1 pathway alone.
Meloxicam falls within the COX-2 preferential category of NSAIDs, meaning it is not COX-2 specific. At higher doses, its focus on only the COX-2 pathway is diminished. This means that at higher doses, effects on the gastrointestinal tract, kidneys, and blood clotting mechanisms can still be affected.
Also Read: What Can You Give A Cat For Pain? 6 Vet-Recommended Options
What Does Meloxicam Do for Cats?
Beyond a single injectable dose for short-term pain relief, continued use of oral meloxicam is under debate.
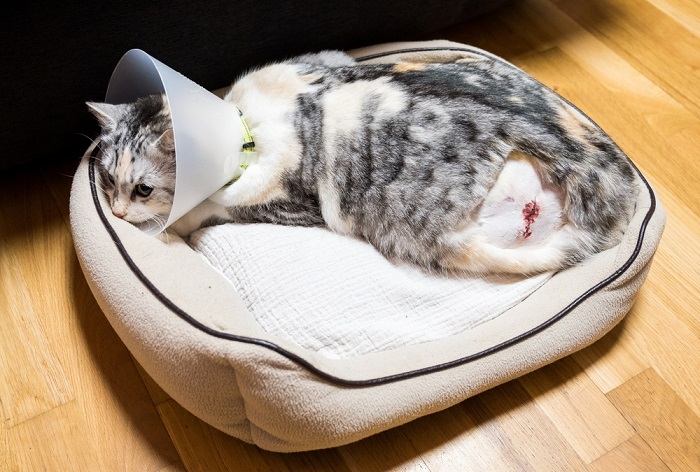
Injectable meloxicam is FDA approved for use in the United States for short-term relief of pain and inflammation in cats, especially for post-operative pain and inflammation associated with surgeries like ovariohysterectomy (spay), castration (neuter), and orthopedic surgery.
Often, an injectable dose may be given by a veterinarian the same day as a surgical procedure or other case where pain and inflammation is present.
Also Read: How To Keep Your Cat From Jumping After Surgery
However, beyond a single injectable dose, continued use of oral meloxicam in cats is under debate. The Metacam oral suspension is only FDA approved in the U.S. for dogs, though it has been used off-label in cats for many years. In some other countries, the oral form of meloxicam is approved for use in cats.
The debate develops from the risks that meloxicam may have on the kidney function of some cats. Compared to dogs, cats appear to be much more sensitive to the COX-1 impacting effects of many NSAIDs, including meloxicam, especially if given for longer periods of time.
Guidelines for very low-dosing of meloxicam have been developed off-label for cats to use for several days. However, even at lower doses, adverse effects have been seen, especially signs of gastrointestinal illness and kidney failure.
In 2010, this prompted both the manufacturer of Metacam (Boehringer Ingelheim) and the FDA to issue a warning stating that repeated use of meloxicam in cats has been associated with acute renal failure and death. The warning further advises against additional doses of injectable or oral meloxicam in cats (beyond the single FDA-approved injectable dose).
This warning, which can be found on the drug insert for the oral Metacam suspension, is stated here:
Warning: Repeated use of meloxicam in cats has been associated with acute renal failure and death. Do not administer additional doses of injectable or oral meloxicam to cats.
However, providing some seeming contradiction to this warning, the International Society of Feline Medicine (ISFM) and the American Association of Feline Practitioners (AAFP) in their consensus guidelines on use of NSAIDs in cats published the same year (2010) contain statements supporting the promise of NSAID use in cats.
These statements include reference to published studies that, while limited in number, show some promise for the medium and long-term use of the COX-1 sparing drug meloxicam in older cats and cats with chronic kidney disease.
A summary of these statements, as provided in Plumb’s Veterinary Drug Manual, is also provided here:
It is only recently that NSAIDs have become licensed for long-term use in cats in some countries. The panel believe that these drugs have a major role to play in the management of chronic pain in cats, but at present only limited feline-specific data are available. To date published studies of the medium- to long-term use of the COX-1 sparing drug meloxicam in older cats and cats with chronic kidney disease provide encouraging data that these drugs can be used safely and should be used to relieve pain when needed. While further data are needed, and would undoubtedly lead to refinement of the guidelines presented here, the panel hope that these recommendations will encourage rational and safe long-term use of NSAIDs in cats, thereby improving patients’ quality of life in the face of painful disease conditions.
To try to clarify their position, the AAFP released this statement shortly afterwards, including some guidelines for veterinarians to follow if considering use of meloxicam in cats:
The AAFP understands that as a result of discussions between the FDA and Boehringer Ingelheim, the following warning has been placed on Metacam, effective September 2010: Repeated use of meloxicam in cats has been associated with acute renal failure and death. Do not administer additional doses of injectable or oral meloxicam to cats.”
The AAFP believes that practitioners should follow this warning, as failure to do so could expose practitioners to liability. Should a practitioner choose to use any drug off label, he or she should:
- Consider the condition of the cat and determine, in his or her professional opinion, if off-label use is warranted.
- If there is an alternate approved drug, practitioners should consider utilizing that drug.
- Practitioners should obtain written owner consent prior to off-label use. Consent should include discussion of warnings included in package inserts.
- State licensing boards may have specific regulations covering extra-label use, and you should consult with your State VMA regarding any regulations that may exist in your State.
The AAFP wishes to clarify that when it co-produced the Long-term Use of NSAIDs in Cats guidelines with the ISFM, the above warning label associated with the use of Metacam in cats (the guidelines were published in July 2010) was not required, thus the warning was not noted in the guidelines regarding use of Metacam.
The essential summary here is that continuing meloxicam beyond the first single injectable dose carries with it significant risks, especially to cats with underlying kidney disease. Off-label use can still be considered in some cases, but has to be weighed heavily against the risks.
In 2011, Onsior (robenacoxib) was approved by the FDA after being introduced in Europe in 2009. In cats, an injectable dose can be followed by additional oral doses for a total of three days of therapy. Onsior has been demonstrated to be much safer to use in cats, and so has largely replaced meloxicam as a post-surgical NSAID.
Also Read: 10 Subtle Signs Your Cat May Be Sick
Side Effects of Meloxicam for Cats

Despite the warnings against continued use of meloxicam, a single injectable dose (which is FDA approved for cats) appears to be relatively safe.
It’s important to note that while there are many precautions against continued use of meloxicam in cats, a single injectable dose (which is FDA approved for cats) appears to be relatively safe.
For the injectable dose, some cats demonstrated a blood urea nitrogen (BUN) elevation, low red blood cell count, and discomfort at the injection site in field studies.
In other cases, meloxicam has also caused GI effects like vomiting, diarrhea, and poor appetite, as well as behavior changes and lethargy.
The manufacturer warns that additional doses (beyond a single approved injectable dose) whether oral or injectable is contraindicated in cats, and the FDA warns against repeated use in cats.
Here again is the warning that can be found on the drug package insert for Metacam:
Warning: Repeated use of meloxicam in cats has been associated with acute renal failure and death. Do not administer additional doses of injectable or oral meloxicam to cats.
However, it is only fair to note that meloxicam is licensed in some countries for low-dose long-term use suggesting that benefits may outweigh risk in some cases.
As many as 40% of cats over the age of 10 may have chronic kidney disease present according to the ISFM. However, it may not be overly apparent to a pet parent that kidney disease is present when in its earliest stages as many cats may eat, drink, eliminate, and behave normally.
This is the main reason why precautious use of NSAIDs in cats is such a concern. NSAIDs should not be considered in cats at all unless a recent lab work panel, including a urine sample, has been collected to assess renal function.
Safe use of meloxicam has also not been established for cats younger than 4 months of age.
If you are ever concerned that your cat may have developed adverse reactions while using meloxicam, or if your cat accidentally ingests meloxicam intended for your dog, make sure to contact your veterinarian, the ASPCA Animal Poison Control Center (1-888-426-4435), or Pet Poison Helpline (1-855-764-7661) immediately for further advice.
Also Read: Drug Poisoning In Cats: Causes, Symptoms, & Treatment
Meloxicam for Cats Dosage

There are many risks associated with continuing meloxicam in a cat beyond the single injectable dose that is typically given at a veterinary practice.
For these reasons, no dosages for meloxicam for cats can be provided here. All doses in the U.S. are considered extra-label and should only be provided through an attending veterinarian.
If you live in a country where meloxicam is approved for long-term use in cats, it is very important to follow your veterinarian’s instructions, as low dosing protocols have been described associated with those approvals. Sometimes, this involves only giving a dose once every two or three days.
If you live in the U.S., there are two important things to keep in mind. First, meloxicam is available and FDA-approved for use in dogs, meaning that some cat owners who also have a dog may have this drug at home. If you have this drug at home for your dog, it should never be given to your cat, especially not without discussing it with your veterinarian first. There are other drugs that can be considered for both inflammation and pain before use of meloxicam.
Also Read: Homeopathy For Cats: What You Need To Know
Second, it’s important to understand that it is not illegal to prescribe meloxicam to cats in the U.S. However, it is considered an off-label application of the drug to prescribe to a cat. Many drugs in veterinary medicine are prescribed this way. Prescribing a drug off-label requires that a veterinarian has been in close communication with a pet parent and has close knowledge of the cat patient, including a recent examination.
With these steps in place, meloxicam could be prescribed using a low-dose protocol as long as the risks and benefits have been discussed and the benefits appear to outweigh the risks. Some veterinarians may require a release form or similar document to be signed to document that these discussions took place, in the event that adverse effects are seen.
In Summary

Though meloxicam is a useful drug that targets ability pain and inflammation, in cats, there are significant safety concerns in its use beyond a single injectable dose.
Meloxicam is a very useful NSAID in terms of its ability to combat pain and inflammation. However, in cats, there are significant safety concerns in its use beyond a single injectable dose. In the U.S., continued oral administration of meloxicam is considered contraindicated, and the manufacturer of Metacam also warns against continued use.
There may be some situations where off-label use of meloxicam may be warranted in which case the lowest, least frequent dose that manages signs of illness should be used. It is on this basis that meloxicam does carry approvals for long-term use in some countries.
Drug Dosing Disclaimer: We are only able to provide doses for medications that are FDA approved for use in cats and only as the label guidelines dictate. For medications that are used off-label we can only provide guidelines and safety information for use. Safe and appropriate dosing for off-label medications can only be determined by a primary care veterinarian.
We encourage you to work with your veterinarian to determine if a particular medication is appropriate for your cat. Changing or adjusting a dose for your cat on your own without consulting with a veterinarian can carry risk. We do not encourage use of medications prescribed for human use in pets without first consulting with a primary care veterinarian.
Frequently Asked Questions
What does meloxicam do for cats?
As a nonsteroidal anti-inflammatory drug (NSAID), meloxicam has the ability to block signals of pain caused by inflammation in the body.
Meloxicam may commonly be used in cats as a single injection following a surgical procedure like a spay, neuter, or orthopedic (bone/joint) surgery where lots of inflammation and pain may be present.
Due to significant safety concerns, continued use of meloxicam beyond one day either with further injectable or oral doses of the medication is considered contraindicated in the United States, as well as by the manufacturer of the brand Metacam (meloxicam), Boehringer Ingelheim.
How much meloxicam do I give my cat?
Since 2010, the oral suspension of Metacam has carried the following warning:
Warning: Repeated use of meloxicam in cats has been associated with acute renal failure and death. Do not administer additional doses of injectable or oral meloxicam to cats.
Continued use of meloxicam beyond a single injectable dose is considered contraindicated by both the manufacturer and the Food and Drug Administration (FDA).
Oral meloxicam should not be given to cats because of the significant risk of gastrointestinal effects and kidney failure.
Meloxicam does carry approval for use in cats at very low doses in some countries. If you live in one of these countries, or if your veterinarian has prescribed meloxicam to your cat, it is very important to only seek advice on dosing from your attending vet.
If you have meloxicam at home for your dog, never give your cat a dose of this medication without first consulting with your veterinarian, who may have alternative recommendations.
When should I give my cat meloxicam?
In short, you should never give your cat meloxicam due to the significant safety concerns that exist for administering meloxicam for any length of time.
If you live in a country where meloxicam is approved for long-term use in cats, it is important to discuss any questions about when to give it with your veterinarian.
How long can a cat stay on meloxicam?
Safety for use of meloxicam in cats has been established for a single injectable dose, which is typically given at a veterinary practice on the day of a surgical procedure or other situation involving pain and inflammation where use of the injection is warranted.
Beyond that single dose, no truly safe dose for meloxicam for cats has been established, and since 2010, repeated use of meloxicam in cats has been considered contraindicated by the manufacturer.
There are some protocols at low doses that describe use for several days, however health concerns may still be seen even with low or infrequent doses, especially for cats with underlying kidney disease or dysfunction.








This medication was given to my cat and the Vet practically gave the dosage as overdose. On the packaging from the Vet’s label was indicated to give 0.6 mL to a cat 17 years old with a diagnosis over early kidney disease from the blood test. Unfortunately we followed the Vet’s instruction because we trusted his orders although I was wandering why wasn’t I warned about possible sever life threatening side effects. My loving Felix died after 3 days of receiving 0.6 mL of the medication every 24 hours. I’m devastated because I feel like my cat was murdered
Hi Lilian,
I’m so sorry to hear of the sudden and tragic loss of Felix. I can tell you feel justifiably hurt and angry. I could work out the volume you mention to make sense for one of the traditional dosing protocols, at least with the lower concentration of meloxicam. Unfortunately, any dose, even the lower ones can still be a risk. I don’t know all the circumstances, and there are veterinarians who are comfortable using meloxicam, but I can only agree that these risks should be fully discussed when considering use of it.
Thank you Dr. Chris Vanderhoof for your response, I tried to reply to you but it seems this links is not working properly. I would appreciate you helping understand if the dosage was correct, because in my understanding now it looks like Felix was overdosed
Thank you Dr. Chris Vanderhoof, I appreciate your response. Felix was brought into the Vet last Thursday because he was limping and after blood test and x-ray was made we were told from our Felix Vet he will decide which treatment would be possible once the blood test confirms Felix hasn’t any kidney problems. We were NOT informed about any risks of the treatment just that it would help with the inflammation of Felix back left knee to go down possibly and then go from there. We took Felix home and on Friday morning we went back to the Veterinary station to first consult with the Vet the results of the blood test findings but Felix Vet wasn’t available so another Vet handed over the medication. I wanted to discuss the blood test results which was important to understand the risk of the treatment and discuss about possible side-effects if there’s known about but the Vet who was available on Friday didn’t want to get much involved and said he was only going to handle over the medication and regarding the blood test results or anything else I can discuss with the Vet who was on Felix treatment on Monday. Practically we were helpless because we wanted to understand about the medication if it was safe and obviously the Vet who was available and the Vet assistant also confirmed that the dosage was to follow what was written on the label sticked to the box therefore, because we wanted to see Felix improving we in faith trusted what we were told to do. Unfortunately there was nothing else discussed about giving the medication with food to prevent possible side-effects nor was discussed the possible sever threatening side effects. Felix 17 years and five months old, his weight was 5.85 kg. Details about the treatment/medication on the medication box is showing Active Constituent: 0.5mg/mL MELOXICAM. On the bottle of 15mL is indicated initial Dose 0.1mg/kg body weight. Maintenance dose 0.05mg/kg body weight. Practically we were ordered to use the dosage indicated on the label and that was – administrate once daily 0.6mL every 24 hours. From Friday evening to Sunday evening Felix was given that dosage of 0.6mL with a oral syringe every 24 hours. Monday morning Felix around 11.30 am started showing signs of tongue moving rapidly in his mouth and was Meowmy very loud, it lasted 3 minutes then he was stable but still was looking sick. Although Felix since Friday did eat, drink and clean himself regularly and managed to enter that cat litter but only to pee, not poo which was already uncommon from him already was concerning me therefore, I called our Vet praxis to let them know that I would bring Felix in, but I was told from the receptionist that all Vets were too busy too check on Felix and if I didn’t want to wait until 4.00pm and the situation looks urgent I should go to an emergency Vet station and that’s what we did. Once there Felix was handled by 2 Vets and his heart was beating so fast that he was put under oxygen. I Don’t understand why at the emergency room the Vet’s didn’t realize that the MELOXICAM could have caused Felix deterioration and try to disintoxicate him by making him throw up the toxicity or atleast confront the possibility he was having a overdose from the treatment, instead they kept advising us to put him to sleep because he was a old cat and even if they would manage to stabilize still he would need to go under other tests to see how he would survive and what the underlying conditions are and still with no guarantee that he would survive. I believe they just thought it would be easier to just put him to sleep so it might no reveal that he was overdosed and that would be because of the wrong information us given, plus we weren’t told about those possible threatening side-effects. As we saw Felix in the oxygen area he recognized us, it was heartbreaking. Minutes later we were asked to leave the room to discuss further if we intend to allow them to put Felix to sleep, strangely 2 minutes later we were told he’s going, he was practically looking like he was dieing and that’s when we decided to allow the procedure to go ahead and let him go without suffering even more. Everything went so fast, it was like a nightmare and we couldn’t wake up. That day was the worst day if our life. On Tuesday night I started investigating and that’s when I realized Felix may have been overdosed means the medication dosage was more than he should have gotten plus I started investigating about MELOXICAM and that’s where I came to understand that treatment should not have been allowed without our understanding of the severe side effects whereby if I would have been aware of I would have NOT agreed on that treatment and that’s now killing me inside because I could have prevented his death if only we would have had a proper discussion with our Vet but didn’t occur because he just avoid it happening. It would be great if you could atleast tell me if the dosage was wrong and overdose. Kind regards Lilian
Dr.Chris Vanderhoof I want to remark the last comment from 7 September 6.00am is the correct one, the previous one has some typo errors which I had to edit so ignore the reply to you from tomr showing – 5.10am as it has too many typos errors. Unfortunately I was in a hurry and can happen but because to avoid misunderstanding I replied again making sure the comment was correctly showing. Kind regards Lilian
Thank you Dr. Chris Vanderhoof, I appreciate your response. Felix was brought into the Vet last Thursday because he was limping and after blood test and x-ray was made we were told from our Vet he will decide which treatment would be possible once the blood test confirms Felix hasn’t any kidney problems . We weren’t informed about any risks of the treatment just that it would help with the inflammation of Felix back left knee to go down possibly and then go from there. We took Felix home and on Friday we went back to the Veterinary station to first consult the results of the blood test findings but our Vet wasn’t available so another Vet handed over the medication. I wanted to discuss the blood test results which was important to then understand the risk of the treatment, but the Vet who was available on Friday didn’t want to get much involved and said I’m here only to handle over the medication and regarding the blood test results you can see your personal Vet on Monday. Practically we were helpless because we wanted to understand about the medication if it was safe and obviously the Vet who was available and the Vat assistant all confirmed that the dosage was to follow what was written on the label sticked to the box. So because we wanted to see Felix improving we in faith trusted what we were told to do. Unfortunately there was nothing else discussed like giving the medication with food to prevent possible side-effects nor was discussed the possible sever threatening side effects. Felix was 5.85 kg and on the medication box is showing Active Constituent: 0.5mg/mL MELOXICAM. On the bottle of 15mL is indicated initial Dose 0.1mg/kg body weight. Maintenance dose 0.05mg/kg body weight Practically we were ordered to use the dosage indicated on the label and that was administration once daily 0.6mL every 24 hours. From Friday to Sunday to Felix was given that dosage with a oral syringe. On Monday morning Felix around 11.30 am started showing signs of tongue moving rapidly in his mouth and was Meowmy very loud, it lasted 3 minutes then he was stable but still was looking sick. Although Felix did eat, drink and clean himself regularly and managed to enter that cat litter bit only to pee, not poo which was already uncommon from him. I called our Vet praxis to let them know that I would bring Felix in, but I was told from the receptionist that all Vets were too busy too check on Felix and if the situation looks urgent I should go to an emergency Vet station and that’s what we did. Once there Felix was handled and his heart was beating so fast that he was put under oxygen. I Don understand why at the emergency room the Vet’s didn’t realize that the MELOXICAM could have caused Felix deterioration and try to disintoxicate him by making him throw up the toxicity or atleast confront the possibility he was having a overdose from the treatment, instead they kept advising us to put him to sleep because he was a old cat and even if they would manage to stabilize still he would need to go under other tests to see how he would survive and what are the underlying conditions but still with no guarantee that he would survive. I believe they just thought it would be easier to just put him to sleep so it might no reveal that he was overdosed. As we saw Felix in the oxygen area he recognized us, it was heartbreaking. Minutes later we were asked to leave the room to discuss further if we intend to allow them to put Felix to sleep, strangely 2 minutes later we were told he’s going, he was practically looking like he was dieing and that’s when we decided to allow the procedure to go ahead and let him go without suffering more. Everything went so fast, it was like a nightmare and we couldn’t wake up. That day was the worst day if our life. On Tuesday night I started investigating and that’s when I realized Felix may have been overdosed means the medication dosage was more than he should have gotten plus I started investigating about MELOXICAM and that’s where I came to understand that treatment should not have been allowed without our understanding of the severe side effects whereby if I would have been aware of I would have agreed on that treatment and that’s now killing me inside because I could have prevented his death if only we would had had a proper discussion with our Vet. It would be great if you could atleast tell us if the dosage was wrong and overdose. Kind regards Lilian
Thank you Dr. Chris Vanderhoof for your response, I tried to reply to you but it seems this links is not working properly. I would appreciate you helping understand if the dosage was correct, because in my understanding now it looks like Felix was overdosed
Hi Lilian,
Thank you for sharing more information. I certainly recognize that these events were very sudden and tragic for you, and something acutely happened to Felix a couple days after starting the meloxicam. However, I’m a little unclear on what may have actually occurred, but I will look to be as objective here as possible.
The dosing information you provided of the 0.6ml certainly matches a 0.05mg/kg dose based on Felix’s weight of the 5.85kg. This does follow a traditional dosing protocol for cats, and would not support a mistaken dose or overdose specifically. If the loading dose of 0.1mg/kg (which would have been about 1.2ml) was skipped and you just started at the maintenance dose of 0.6ml, this certainly may have actually reduced some risk.
There have been some lower doses described to consider for cats with kidney disease risk. I’m not clear if you found out what Felix’s bloodwork looked like or if there was any kidney disease risk for him.
Unfortunately, as the article indicates, there is always some risk beyond a single oral or injectable dose for cats and it seems to be the case with any dose, even the ones that are commonly accepted, as was the case for Felix’s prescription.
But what you’re describing in terms of what happened to Felix is unclear to me. It sounds like he had acute breathing trouble, but there was no change to eating or drinking habits. You did not mention signs of vomiting either.
Typically, a cat with acute kidney injury would have a poor or absent appetite and vomiting would usually be seen, along with lethargy. It’s not clear if at the ER they provided a diagnosis of what was occurring. This sounds more like a respiratory, heart-related, and/or blot clot type concern based on the acute nature of it, panting/open mouth breathing, high heart rate, and need for oxygen support. This doesn’t match with what I would typically expect as side effects from meloxicam.
Perhaps there was another underlying condition that progressed separately? There certainly could be details I am not aware of or privy to here and perhaps this is an uncommon presentation of meloxicam side effects, but what you’re describing doesn’t follow what I would expect.
It may be possible to reach out to one of the ER vets or get their notes/report from Felix’s visit to see what the diagnosis was suspected to be.
You know kidney failure causes anaemia and respiratory problems due to the lack of haemoglobin being produced?? healthy kidneys produce a hormone that makes red blood cells or platelets that transport oxygen throughout the cats body and if there’s none being made due to kidney damage of course they will have those symptoms its mad how licensed veterinarians dont know this its apalling (sounds like he had acute breathing trouble, but there was no change to eating or drinking habits. You did not mention signs of vomiting either.
Typically, a cat with acute kidney injury would have a poor or absent appetite and vomiting would usually be seen, along with lethargy. It’s not clear if at the ER they provided a diagnosis of what was occurring. This sounds more like a respiratory, heart-related, and/or blot clot type concern based on the acute nature of it, panting/open mouth breathing, high heart rate, and need for oxygen support. This doesn’t match with what I would typically expect as side effects from meloxicam) may I add a cat who has kidney disease just because they don’t vomit doesn’t mean they don’t have it. That’s an outrageous thing to say. If they stop eating its more or less the same thing how can they vomit if they are not even eating?? I know because I’ve had 2 cats die from it. Lillian my heart goes out to you and its mad that licensed veterinarians aren’t even aware of how it can kill it shouldn’t even be on the market full stop only with the exception of using it once. Its crazy how we put our trust in the hands of people who we think know wat they are doing but they haven’t a clue for anyone reading this my heart goes out to you but just remember it wasn’t your fault and for anyone who disagrees the day you get a cat and go through wat I did is the day you’ll research and learn far more than any of the licensed veterinarians are even aware of because simply put it happened to you.
Hi Marina,
I am fully aware that kidney failure causes anemia. And that in cases of severe anemia you can certainly have respiratory concerns because of the lack of circulating hemoglobin and resultant oxygen depletion. However, this is not an effect that occurs immediately or with an acute kidney injury following a single toxic insult to the kidneys. This is an effect we will see over time with chronic kidney disease progressing into kidney failure or in cats who have been in kidney failure for some time. I have seen plenty of cats with acute kidney injury or acute kidney failure with completely normal CBCs. You may see some breathing changes in cats that are in severe acidosis because of kidney failure who are trying to compensate but this does not usually mimic progressive respiratory distress to the point of requiring an oxygen cage.
And despite your clear belief to the contrary, an acute kidney injury causing signs this severe could not occur without GI signs as well. The toxic effects of high azotemia in acute kidney failure will at the least suppress appetite, which did not occur with Felix when the breathing concerns started as he was clearly seen to still be eating. And yes, cats can most certainly vomit with no food in their stomach. If a toxic effect is significant enough, they may only vomit bile or just dry heave, but food in the stomach is not required for vomiting to occur.
You clearly had a poor experience with your own cats and for that I am truly sorry. But experience with personal pets does not mean that experience is widely applicable to everyone else’s pets and their health conditions.
Don’t presume that experience limited to personal pets and googling a topic gives a better understanding of physiology, disease, and medicine than a trained and experienced doctor. We have to think in a far more comprehensive and unbiased way, though I admit we are not always the best at communicating our thought process and rationale and I think we could all do a great deal better at communication and education, so that people don’t feel the need to get their information elsewhere and arrive at poorly-informed conclusions.
I do believe there were clear missteps that occurred in Felix’s care, especially with poor communication and follow up. I also believe that meloxicam carries significant safety risks for cats that should always be discussed if it’s being prescribed and my article doesn’t shy away from that opinion.
But while meloxicam may have been related, there at least is not enough evidence to say that for sure because we don’t even have bloodwork result information to confirm kidney failure was present. All we have is a sudden onset of acute, quickly progressing respiratory distress. The way the ER team approached things, it seems they were more concerned about a different underlying cause.
Doctors cannot have tunnel vision or bias when assessing cases and we have to entertain all possibilities. I don’t care much for meloxicam use in cats but even though I hold that opinion, to say with biased confidence that it clearly caused these effects would be very inappropriate as there are plenty of other potential causes that have to be considered as well.
My vet here in Europe told me to use Metacam for oral use after my cat’s tooth surgery. Due to complications of the stitching getting undone etc. we’re now on week 3 of the (by the manufacturer) recommended 2 weeks of use and I’m starting to have doubts. A friend of mine works in a 24/7 vet clinic and told me about how many cats they see dying on their very emergency tables due to liver failure after long term usage of oral Metacam.
When I try to tell my vet about it, they encourage me that nothing will happen because they have several cat patients that have been administered daily oral dosages of Metacam for years now.
I want to believe my vet, but my friend and her colleagues have persuaded me to please disregard my vets advice for the safety of my cat.
Since oral use is not approved in the US, I cannot seem to find any source that would be impressive enough for my vet to take me seriously.
But having read the comorehensive article and some of the comments, I definitely feel encouraged to go fight for my cat’s well-being.